The Surprising Reason I Gave Up Veganism After 6 Years


When I told my parents nearly seven years ago that I had decided to adopt a vegan diet, the declaration instigated an argument that ultimately ended in a vow from me. "I'll only do this as long as it serves my health," I told them, adding that I'd make good on the promise with regular blood testing to monitor my nutrient levels. I still remember the haughtiness that flashed through me as I appeased them. I was several weeks into my new lifestyle and feeling so energized—so well—that I couldn't imagine this hypothetical dilemma ever crossing into reality. For the first time in three brutal years, I finally felt empowered rather than controlled by food.
My parents weren't wrong to be concerned. I was in tentative recovery from my eating disorder at the time, and any kind of restrictive diet was bound to raise red flags. But veganism would ultimately become the first life raft I found during that impossible chapter in my life, as it taught me to listen to my body and find gratitude in the food I was consuming. With every nourishing meal—crafted around seasonal produce sourced from my local farmers market—I realized I was piecing myself back together.
Over the next several years, I'd come to use the terminology "plant-based" instead of "vegan." I learned more about the ethical and environmental ramifications of our global food systems. I climbed out of recovery into a mostly comfortable remission. But the evolving circumstances around my way of eating only bolstered my enthusiasm for it.
Then, at the beginning of this year, I was forced to confront the sole non-negotiable I had so naïvely thought I'd never have to face. After several weeks of feeling consistently drained, moody, and just generally "off"—all while maintaining my otherwise healthy lifestyle—I knew it was time to consider that perhaps my diet was playing a role.
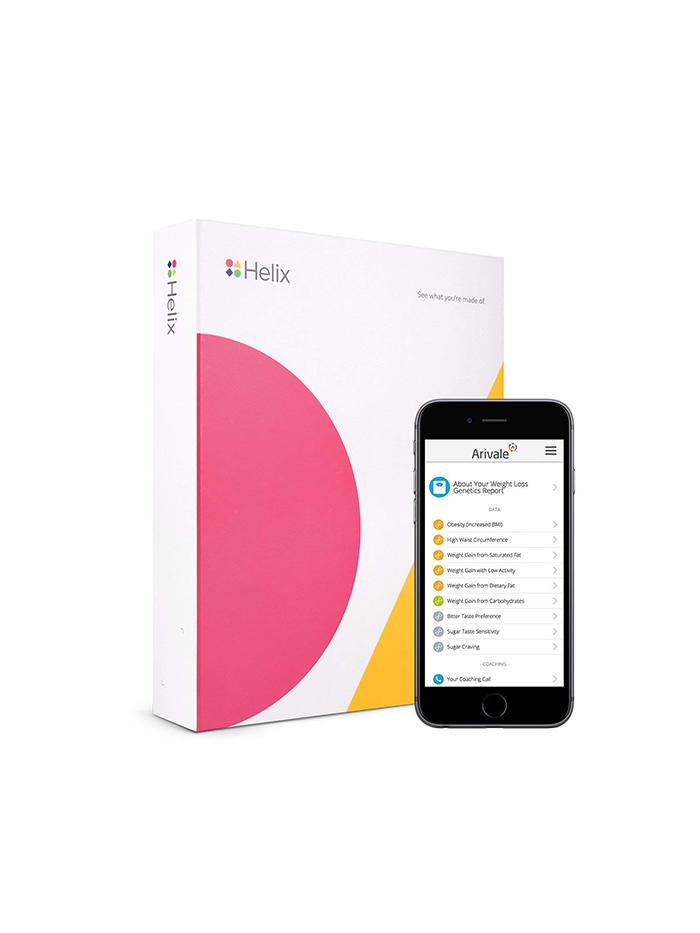
Ultimately, that would mean following my own protocol and undergoing blood testing with Arivale, a personalized wellness program that utilizes nutritional, genetic, and hormonal markers to navigate your way to optimal health. But first, I found myself toying with a more unscientific strategy: cravings.
It all started with eggs

Months before I sent in my first blood samples to Arivale's lab, I went to brunch one chilly Saturday morning at Sqirl, one of L.A.'s best farm-to-table restaurants. Faced with a menu I've perused many times, I suddenly felt an intense craving for a runny egg atop my usual grain bowl. The knowledge that the café only sources the most sustainable ingredients made the decision an easy one, and within minutes, I was breaking the sunny yolk over my kale: my first egg in six years. On the way home, I stopped by farmers market and bought a dozen more.
I'm not going to pretend that this official break in my plant-based diet after that revelatory breakfast was due to a spontaneous burst of energy or any physical benefit, for that matter. It just tasted that good, and I reasoned that so long as I continued to abide by my philosophy of eco-friendliness, there was no reason I shouldn't see if re-adopting eggs into my diet made any eventual impact.
I wouldn't have to wait long to find out: Within a few days, my energy levels soared, I felt sharper throughout the day, and my workouts even felt easier. It was incredibly gratifying to feel so much better so quickly—so that even though it was bittersweet to take a step away from a way of life I had followed for years, I knew it was the right decision.
Besides, it was only eggs. I had no intention of adding anything else back to my diet—that is until I learned about Arivale several weeks later.
When I sat down with Arivale co-founder Clayton Lewis last March, I was curious but skeptical. I had tried a few different at-home genetic wellness tests at that point, only to find the margin of error far too wide for my comfort. (This became most evident when one claimed I had a high sensitivity to avocados, which was as ludicrous as it was horrifying.) But as Lewis continued to explain it, Arivale seemed a bit different. For one thing, all blood testing is done in a lab—no shoddy at-home finger-pricking necessary. In addition to testing my nutrient levels, they'd dive into genetic markers spanning diet, fitness, and general health. My cortisol levels would be monitored. Once I got my results, I'd work with a health coach over the course of six months to address any necessary changes.
Arivale prides itself on its comprehensiveness, and that felt painfully evident as a nurse practitioner removed eight vials of blood from my right arm a couple of weeks after my meeting with Lewis. But I felt my inner health nerd activate, and by the time my results were available to discuss with my health coach, a registered dietitian named Erica, I was practically feverish with anticipation.
It was fascinating, to say the least, to parse through all the different panels with Erica—to see, in concrete detail, all the small ways I could easily make myself feel better. I learned that my cortisol levels were slightly off-kilter, for example, so we immediately set a goal to reduce my coffee intake and manage my stress. I learned that I have an increased genetic risk for certain joint and tendon injuries, which validated my commitment to low-impact exercise like yoga. I even learned that I am genetically predisposed to be a morning person—no arguments there.
But my enthusiasm faltered slightly as we dove into the nutrition results. Here, I saw in exquisite detail how the diet I had once felt so sanctimonious about was now falling short. My iron levels were borderline. I was deficient in vitamin D, despite my Southern California lifestyle. Most interestingly, my omega fatty acid levels indicated that I was exposing my body to a ton of inflammation—something that my egg intake wasn't necessarily helping.
The Omega-6–to–Omega-3 Ratio
"Fatty acids" is such a buzz phrase that it actually oversimplifies an important distinction between two key types. Research tells us that our ratio of omega-3 and omega-6 fatty acids has a serious impact on our general well-being: A diet too heavy in omega-6s is linked to obesity, metabolic syndrome, and general inflammation. The problem is that our modern diet heavily emphasizes omega-6 fatty acids, which are found in eggs, meat, and vegetable oils. Omega-6s are important to our health in small amounts, but a counter-balance of omega-3s—the healthy fats found in fish and nuts—keep that inflammatory response in check.
I had confided to Erica that though my energy levels were significantly higher after incorporating eggs into my diet, I was still struggling a bit with my mood and general brain fog. While my off-balance cortisol levels were certainly a likely culprit, Erica noted that my low omega-3 levels could also be playing a role: My blood panel indicated that my ratio placed me squarely in the red for increased inflammation. And because omega-3 fatty acids—and more specifically, EPA and DHA—are so essential for brain health and development, studies show that a deficiency can exacerbate mild depression, in addition to other mood-related symptoms like fatigue.
Erica was aware of my mostly vegan diet, so she ultimately prescribed me an omega-3 supplement as well as a prenatal vitamin (which are rich in DHA). While she was confident that we could make a difference in my levels by supplementation alone, she did note that I would have the most immediate and obvious success with some changes in my diet. I cheerfully replied that I was optimistic about the supplements but found myself silently vowing yet again that if I didn't feel better in the coming weeks, I'd try something different.
A poke bowl a day…

Despite my terrible record of remembering to take vitamins on a daily basis, my enthusiasm for my new lifestyle won out and I took my supplements as prescribed. But consistency wouldn't ultimately be the problem. Instead, I found myself feeling debilitatingly nauseous after taking my pills each morning—often to the point of pulling over during my morning commute. Certain tweaks like taking them on a full stomach or taking them later in the day had little effect. Soon, I realized that it wasn't worth it to be feeling worse than I had been before.
Frustrated, I departed on a trip to Aruba with the hope to spike my low vitamin D levels at the very least. Then, out of "respect for local cuisine" but really out of sheer desperation, I ordered fresh tuna for lunch. I had officially crossed back over the threshold I had left behind so many years ago, and it felt both entirely wrong and so very right.
After returning home, I started to experiment with incorporating a few servings of sustainably sourced seafood into my weekly diet. I learned to cook salmon for the first time in my life. I began adding a scoop of ahi tuna to the poke bowl I frequently order for lunch. I remembered how much I love oysters. I realized how much fun it was to be opening my diet up to a host of new ingredients. Then I realized that perhaps it wasn't just the novelty of the food that was putting me in such high spirits, but the food itself.
Over the next several weeks, I reveled in the significant changes I felt physically and mentally. My brain fog all but lifted; my energy levels peaked. I felt more motivated to engage consistently in the self-care rituals that mitigate my stress, like hiking, journaling, and prioritizing general "me" time. Being in a good mood felt less and less like work until one day I realized I was no longer scanning for potential stressors to undermine it all.
But my inner skeptic—the quiet but persistent voice that wondered if this was all the result of a very convincing placebo effect—wouldn't be totally silenced until my second round of blood tests came back. During our final call together, Erica and I marveled at how much improvement the results showed from just six months prior. My omega-6 was back in the green. My omega-3, while still not totally optimal, was nonetheless on the rise. Even my iron and vitamin D levels were in the normal range again.
It was immensely validating, of course, to know for sure that my dietary changes had made such a significant impact on my well-being. But I didn't anticipate the wave of emotion that overcame me as Erica and I talked through the results. Here it was, concrete evidence that my vegan diet was no longer serving me. Nine months after eating that first poached egg, I was finally, officially, closing that door—leaving behind not only a way of eating I had held dear but also the girl who had clung to it for survival.
I also have to credit her for the maxim that I've carried with me into this new phase of life—something to be applied not only to my diet but also to every aspect of my wellness routine: "I will only do this as long as it serves my health." This time, I really believe it.
Next up: Why "you look skinny" doesn't feel like a compliment.
Disclaimer
This article is provided for informational purposes only and is not intended to be used in the place of advice of your physician or other medical professionals. You should always consult with your doctor or healthcare provider first with any health-related questions.
-
 Bella Hadid and Gwyneth Paltrow Apparently Love Sakara Life, so We Tried It for 30 Days
Bella Hadid and Gwyneth Paltrow Apparently Love Sakara Life, so We Tried It for 30 DaysHere are our honest thoughts.
By Erin Jahns
-
 The 6 Warning Signs You're Not Getting Enough Protein
The 6 Warning Signs You're Not Getting Enough ProteinAnd what to eat to up your intake.
By Sarah Yang
-
 Everything This Professional Ballet Dancer Eats to Fuel Her for Performances
Everything This Professional Ballet Dancer Eats to Fuel Her for PerformancesHer grocery staples include high-quality French butter.
By Candice Aman
-
 These 8 Foods Are the Worst for Rosacea—Here's What to Eat Instead
These 8 Foods Are the Worst for Rosacea—Here's What to Eat InsteadControl those flare-ups.
By Sarah Yang
-
 15 Things That Cause Bloating and How to Get Rid of It ASAP
15 Things That Cause Bloating and How to Get Rid of It ASAPTry these.
By Sarah Yang
-
 Is the Alkaline Diet Overhyped? What Experts Want You to Know
Is the Alkaline Diet Overhyped? What Experts Want You to KnowHere's how it works.
By Sarah Yang
-
 I'm an Imperfect Dietitian and My Key to Eating Healthy Meals Is Convenience
I'm an Imperfect Dietitian and My Key to Eating Healthy Meals Is ConvenienceTake a peek at my weekly grocery staples.
By Candice Aman
-
 Avoid These 6 Foods—They'll Wreck Your Gut Health
Avoid These 6 Foods—They'll Wreck Your Gut HealthWhat to eat instead.
By Sarah Yang